What to consider when choosing a health plan for your business
If you’ve ever spent time comparing health plans, you know no two plans on the market are exactly alike. One carrier alone might have over 50 slightly different plans, and even “standardized” naming conventions aren’t consistent across the board. From network access to deductibles, copayments, and covered benefits, there are a number of factors that influence the cost and perceived value of a given plan.
So, the question is: how can we make it easier for you and your benefits advisor to compare small group health plans and choose the right one for your business?
The first step is to understand that the value of a plan can’t be represented by numbers alone. For small groups in particular, a truly valuable assessment of any plan should focus on balancing your costs with the preferences, needs, and cost considerations of your employees.
Download the e-book: Annual Renewal Guide
To help you assess the value of a given plan, we’ve laid out a few plan aspects and what those differences might mean for a member.
1. Network access
Investigating the network of a given plan is an important place to start when making comparisons. Often, determining the value is more about assessing the right option for an individual employer than a strict across-the-board numbers comparison.
Some factors to consider are:
Is it an HMO or PPO plan?
An HMO (Health Maintenance Organization) plan typically has strong provider access through a Primary Care Provider (PCP) and offers lower premiums and out-of-pocket costs, but a PPO (Preferred Provider Organization) plan offers more provider choice. PPO plans often include access to a nationwide network of providers. They also offer coverage for out-of-network providers (but at higher cost sharing) and typically don’t require referrals from a PCP to see a specialist, though their flexibility comes at a higher cost.
Is the network tiered?
Tiered plans generally group in-network hospitals and providers according to the cost and quality of care when delivered by them. But, different carriers have different methods for tiering. A hospital that one carrier defines as ‘high-tier’ might not be according to another carrier’s definition, so you can’t assume that similarly-named plans or tiers have identical provider and hospital listings.
Comparing tiers within one plan can be difficult as well. Members typically have higher cost sharing for services from a higher-tier provider than they would with a lower-tier provider. This is done to encourage access to lower-cost care and reduce overall costs. But, if the doctors or specialists that employees want to see are in the higher tier, they could end up paying more for those services than they might with a non-tiered plan.
These tiers can also shift from year-to-year, meaning members might see an increase in their cost sharing if their preferred doctor is switched to a higher tier at the start of the new plan year. To counter the downsides of this type of network, a tiered plan may have a lower monthly premium than other plans.
Assessing the value
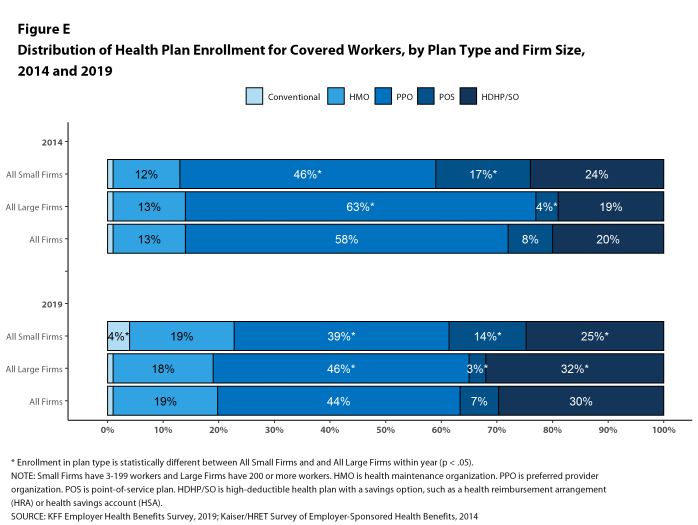
Because of these differences, looking at monthly premiums alone doesn’t tell you everything you need to know about the value of a plan. In fact, despite their higher premiums, PPOs are the most common plan type, with 39% of employees at small firms enrolled in one of these plans compared to 19% for HMO plans, according to the Kaiser Family Foundation 2019 Employer Health Benefits Survey. Access to the doctors and hospitals your employees want is just as important as, if not more important than, the monthly cost of their insurance.
Accordingly, employers should consider where the in-network doctors and hospitals for a given plan are located. If many employees live in one town or region, it’s important to make sure they have convenient access to doctors who can provide regular care.
One factor small employers in particular may want to consider is whether the plan’s network can accommodate their current employees’ medical needs. Employers who are more closely acquainted with their employees may have a deeper knowledge of the services they require.
Given that 55% of US workers have left jobs because they found better benefits at another company, if members of the team heavily rely on services provided by specific hospitals, choosing a plan that includes those locations in its network may be more valuable for retention purposes than other considerations.
2. Member cost sharing
Another point of comparison brokers and employers try to make is with member out-of-pocket costs. But, there’s more to this category than just choosing the lowest number; low costs in one area are often tied to high costs elsewhere.
Deductible
High-deductible health plans (HDHPs) typically have lower monthly premiums, but members are responsible for a greater overall amount of cost sharing before their plan starts to pay. These plans are typically designed to encourage members to search for lower-cost providers and avoid unnecessary use of their plans, which in turn lowers their costs and the costs for their health plan. However, in practice, HDHPs have been found to decrease spending by reducing the use of beneficial services—not just unneeded services.
To make services more affordable when they are needed, many HDHPs also offer a health savings account (HSA) that provides employees with a fund to contribute tax-free dollars to pay for their medical expenses.
Low-deductible health plans come with a higher monthly premium, but, in exchange, members are responsible for a smaller amount of cost sharing. These plans may make the most financial sense for members who have ongoing health care needs and require regular check-ins, procedures, and medications.
Copayments
After the deductible, copayments are another major component of the cost sharing calculation. A 2018 America’s Health Insurance Plans (AHIP) survey found that employees say the most important health benefits are preventive care, prescription drugs, and emergency care. To make sure these benefits are accessible for employees, it’s a good idea to review the copayments for primary care provider visits, prescription drugs, and visits to the emergency room.

Source: AHIP, The Value of Employer-Provided Coverage
For prescription drugs in particular, most plans have tiered pharmacy programs. These pharmacy programs sort covered prescription drugs from lower to higher-cost medications, with generic drugs often found in tier 1 and brand name or specialty drugs located in the highest tiers. Typically, if a drug is in a higher tier, the copayment will also be higher.
Different plans can also have different numbers of tiers, with 3, 4, and 6 being the most common configurations. For that reason, it can be difficult to directly compare pharmacy benefits between plans, as a given drug may fall into a different tier depending on the plan.
But, without getting into specific drugs, it generally makes sense to compare the cost sharing of the highest and lowest tiers when trying to decide which plan has the better value.
Out-of-pocket maximum
Knowing the out-of-pocket maximum (OOPM) for a plan will tell you the absolute highest amount that an employee will pay in cost sharing for covered services during the benefit year. Plans with a higher monthly premium will typically have a lower out-of-pocket maximum. More medically needy employees will benefit from a lower OOPM, as their plans will begin to pay for 100% of covered services earlier in the plan year.
Plans with a high out-of-pocket maximum are typically more affordable on a monthly basis, but could leave members struggling to pay for their medical expenses if they have an unexpected illness, disease, or injury that requires ongoing care.
3. Programs and service
While the network and cost sharing are the most prominent aspects to consider when choosing a health plan, there are always more factors that can contribute to the overall value. Here are a couple things to keep in mind that may not be the deciding factor when it comes to which plan is best, but are worth thinking about as you do your assessment.
Features and programs
Many plans offer additional features that can help employees live healthier lifestyles, get convenient access to care, and save money on certain services. Some high-value programs to look for are:
![]()
Telemedicine. With 66% of Americans now willing to use telemedicine services, virtual care programs are becoming more and more popular. Telemedicine services can benefit employees by encouraging them to get care when they might not otherwise have the time or means to see a doctor.
![]() Wellness programs. As the workplace wellness trend increases in popularity, more plans are offering no-cost wellness programs to help members evaluate and improve their health. These wellness programs also benefit small businesses by improving productivity and creating a more positive company culture.
Wellness programs. As the workplace wellness trend increases in popularity, more plans are offering no-cost wellness programs to help members evaluate and improve their health. These wellness programs also benefit small businesses by improving productivity and creating a more positive company culture.
![]() No cost services. Insurers already offer preventive care at $0 cost sharing, but more and more are starting to offer this same benefit for other, non-preventive services. These programs make it easier for members to access care they might otherwise avoid due to cost, and help members get the medications they need for chronic disease management.
No cost services. Insurers already offer preventive care at $0 cost sharing, but more and more are starting to offer this same benefit for other, non-preventive services. These programs make it easier for members to access care they might otherwise avoid due to cost, and help members get the medications they need for chronic disease management.
![]() Fitness and weight loss benefits. Many plans now offer reimbursements for members who have gym memberships or are part of a weight loss program. Getting money back for working out and eating healthy can be a great way to reward members for what they already do to stay well. It can also help encourage those who might be considering joining a gym or making a change to their diet.
Fitness and weight loss benefits. Many plans now offer reimbursements for members who have gym memberships or are part of a weight loss program. Getting money back for working out and eating healthy can be a great way to reward members for what they already do to stay well. It can also help encourage those who might be considering joining a gym or making a change to their diet.
Customer service
Because health care is so complex, it’s helpful and often necessary to contact customer service and speak with a real person about benefit or claims information. If a carrier’s customer service is unhelpful or unresponsive, that process just got a lot more frustrating for members.
It’s a good idea to ask your benefits advisor about the reputation of a carrier’s customer service team and make sure the insurance provider is going to be a helpful resource for your employees, rather than a pain point. For example, do they offer performance guarantees? Looking at publicly shared customer satisfaction or first-call resolution measurements is a good place to start.
Get more guidance on choosing a plan
There’s no way around it: there are a lot of factors that go into health plan pricing. That’s why making 1-to-1 comparisons between plans is so challenging. But, the key to balancing coverage and cost in a way that makes sense for your business and your employees is to know what your team is looking for from their health plan.
 With these considerations in mind, you’re ready to take on all the challenges of open enrollment. If you’re looking for more guidance on how to put these insights into action, we recommend checking out our e-book, Annual Renewal Guide: What you need to make an informed decision about your health plan.
With these considerations in mind, you’re ready to take on all the challenges of open enrollment. If you’re looking for more guidance on how to put these insights into action, we recommend checking out our e-book, Annual Renewal Guide: What you need to make an informed decision about your health plan.
The e-book contains a guide to open enrollment that will walk you through the decision-making process step-by-step. And because understanding employees’ needs is such a large part of trying to decide what plan to offer, the guide also includes a sample survey you can share with your team to get an idea of their needs and preferences.
Get the download now to use with your benefits advisor as you think about your plan choices for the coming year.